Practical Analytic Approaches to Healthcare Challenges
Routinely performing pre-operative testing is a common practice prior to surgery. The American Society of Anesthesiologists (ASA) Task Force defines routine tests as those done in the absence of any specific clinical indication or purpose (i.e. tests intended to discover a disease or disorder in an asymptomatic patient).1 Routine pre-operative testing typically consists of a panel of blood and urine tests, chest X-rays and electrocardiogram. The purpose is to identify any condition that would add risk to the surgery, and to adjust perioperative anesthetic care to mitigate surgical risk or even postpone or cancel surgery.[1] Although pre-operative testing has long been a common practice there is little or no evidence that supports any benefit for “routine testing” before low risk surgery.[2]
Unnecessary pre-operative testing may cause a patient to be subjected to increased cost of surgical care, false positive, or borderline results that lead to further follow-up investigations.2 Follow-up investigations due to false positive results can cause unnecessary psychological and economic burdens, postponement of surgery, and even morbidity and mortality.2 In a cost effectiveness study by the Agency for Healthcare Research and Quality (AHRQ), it was found that routine pre-operative investigations resulted in a delay or cancellation of the planned surgery in about 2% of cases, some changes to anesthetic management in up to 11% of cases, or resulted in a change in surgical procedure in under 1% of cases.2
The components of preoperative laboratory testing considered in this blog were metabolic, general health, and electrolyte panel; urinalysis; blood glucose; serum albumin, creatinine, potassium, and sodium; bilirubin; complete blood count (CBC), hemoglobin, bleeding time, prothrombin time; alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
To study the practice pattern of this pre-operative laboratory testing in low risk surgery cases we used the MedInsight Health Waste Calculator’s evidence-based algorithm which includes the Choosing Wisely guidelines for identifying unnecessary testing for low risk surgical procedures. The analysis was conducted on claims from a large Midwestern commercial health plan for the year 2015. Low-risk surgeries considered in this study include various endoscopic and laparoscopic surgeries, minor gynecology, orthopedic, ophthalmology, and urological procedures including superficial surgeries.
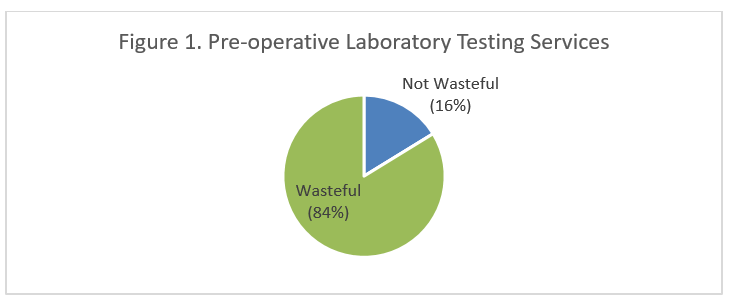
We identified 84 percent of pre-operative laboratory testing services associated with low risk surgical procedures as wasteful, meaning that only 16 percent were necessary (Figure 1). The total aggregate allowed cost for pre-operative laboratory testing was $80,445,931, of which wasteful laboratory testing associated with low risk surgical procedures accounted for $1,471,672, which is 2% of the total cost for pre-operative laboratory testing. These results show that wasteful pre-operative laboratory investigations add significant costs for patients and payers.
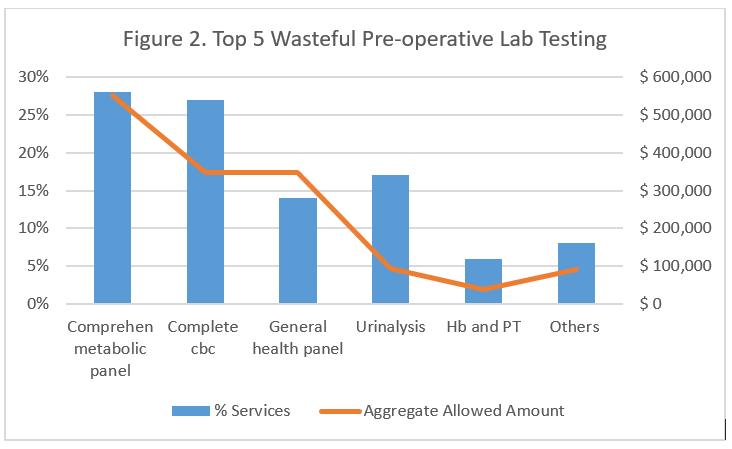
On further analysis of wasteful laboratory testing services, the top five wasteful pre-operative tests based on total cost were comprehensive metabolic panel, complete CBC, general health panel, urinalysis, hemoglobin (Hb) and prothrombin time (PT). Collectively these five common pre-operative lab tests contributed to 92% of the total wasteful laboratory testing. The profiling of these top five pre-operative tests is shown in Figure 2.
It is important to note that claims data alone is not sufficient to identify wasteful services with absolute certainty. However, even with conservative estimates, these findings confirm that a significant percentage of pre-operative laboratory testing done for low risk surgeries are wasteful.
[1] Apfelbaum JL, Connis RT, Nickinovich DG et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012 Mar; 116(3):522–38. [2] Balk EM, Earley A, Hadar N, Shah N, Trikalinos TA. Benefits and Harms of Routine Preoperative Testing: Comparative Effectiveness. Comparative Effectiveness Review No. 130. (Prepared by Brown Evidence-based Practice Center under Contract No. 290-2012-0012-I.) AHRQ Publication No. 14-EHC009-EF. Rockville, MD: Agency for Healthcare Research and Quality; January 2014