With over 77,000 codes, ICD10 diagnosis codes provide a much needed level of granularity for clinicians to use in caring for patients, but they are not particularly useful for large scale analytics. As a result, analysts have developed many different diagnostic groupers to group ICD10 codes into meaningful categories for analysis. Several are available within MedInsight; the MARA risk scores, the Chronic Condition Hierarchical Groups (CCHGs), several available episodic groupers, and our Evidence Based Measures quality metrics.
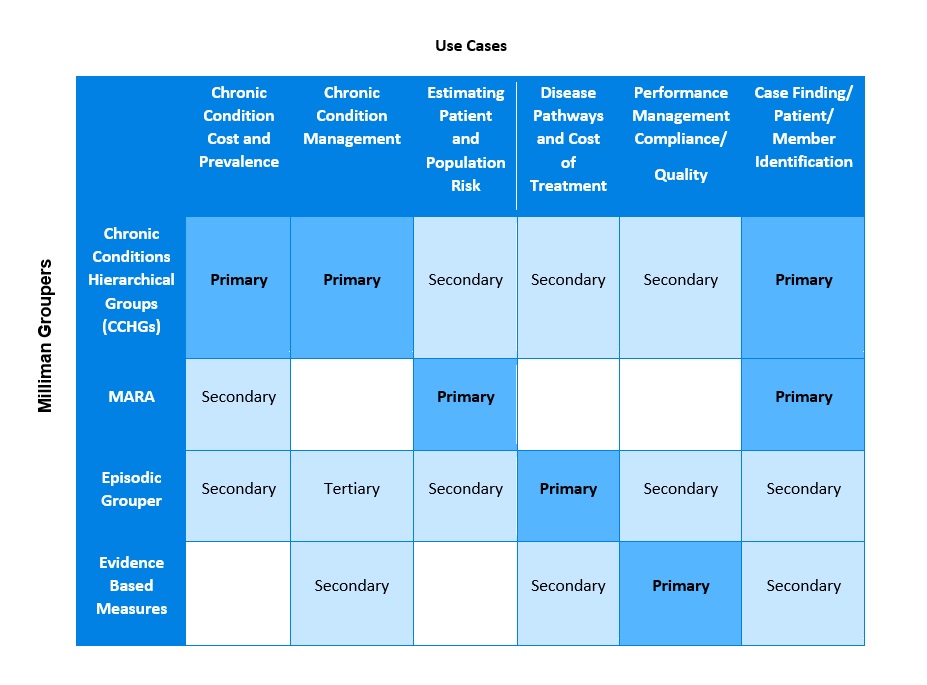
With multiple groupers to choose from, how do you know which one to use? When choosing a grouper, it is important to keep in mind that each grouper is designed to serve a specific primary purpose, so the application or use case for which you need the grouper will be the determining factor in deciding which one will best meet your requirements.
Some of the most common use cases for groupers are chronic condition cost and prevalence analysis, chronic condition management, estimating patient and population risk, disease pathways and cost of treatment, performance management and quality measures, and care management case finding.
We have provided guidance below on the best grouper to use for each indication (called primary) and have identified other groupers that may also be useful for each use case (called secondary).
Chronic Conditions Cost and Prevalence Analysis:
One common use of a diagnostic grouper is tracking chronic condition prevalence within a population over time.
This is often expressed through common questions such as: Do I have more patients with diabetes and hypertension than in the past? Is the increase in treatment costs for patients with cancer increasing faster than the overall population? Is that impacting my bottom line?
These questions can easily be answered by MedInsight’s Chronic Conditions Hierarchical Groups (CCHGs). Because CCHG covers 100% of a patient population and spend, it is designed for population trending over time. The focus on chronic conditions within the CCHGs, and the manageable number of conditions tracked also makes CCHGs ideal for this application.
In the absence of CCHGs, the individual diagnostic categories within the Milliman Advanced Risk Adjusters (MARA) grouper, or an Episodic Grouper could be used similarly as a secondary option.
Chronic Condition Management:
Chronic condition management poses a similar question to the one above on chronic condition cost and prevalence: How well am I managing my pool of patients with a chronic condition?
In this case, CCHGs is also the primary grouper, particularly for measuring the impact of condition management programs and efforts, or fact-checking the impact of an outside vendor program. CCHGs’ embedded hierarchy will filter out other complex conditions, and give you the ability to measure a clinically similar group of members.
Evidence Based Measures can also be useful here to see if compliance rates for recommended care (e.g. HEDIS measures) for patients with chronic conditions are improving.
Episodic groupers can help monitor performance managing procedures and other episodes of care for members/patients with chronic conditions.
Estimating Patient and Population Risk:
For estimating overall population risk, risk-scoring for a physician panel, or any sub-population of patients, MARA is the best grouper to use. MARA’s patient-level concurrent risk score can be aggregated to create a historical risk score to normalize costs across time and between patient populations. The prospective risk score can also be used to predict future risk of a patient or population.
In the absence of MARA, CCHGs can be used to trend population prevalence. The costs to treat patients with chronic conditions over time can provide a good view of population risk over time or point in time risk/chronic condition disease burden for a single patient.
Disease Pathways and Cost of Treatment:
Disease pathways and cost of treatment helps to measure the efficiency of care for a specific condition. Episodic Groupers are the best option when answering questions such as: What is a standard pathway for cancer treatment? Which providers are delivering diabetic care most efficiently?
Evidence Based Measures can also be considered as an additive measure to reflect quality of care in addition to cost efficiency. In the absence of an episodic grouper, CCHGs can add some insight about efficiency by measuring the average cost of a clinically-similar group of patients within each condition group.
Performance Management Compliance and Quality:
Evidence Based Measures are the right place to start when thinking about performance management and quality measures, due to the ability to look at specific compliance with HEDIS or other quality measures. Again, CCHGs can give a good starting point to identify patients with a diabetes and see if they have received an HbA1c, or if your patients with CAD have medication refills if the Evidence Based Measures are unavailable.
Case Finding and Patient/Member Identification:
Finally, to identify patients for chronic condition management programs, the most effective method is to layer groupers together to prioritize patients for evaluation and possible enrollment. CCHGs is used here to zero in on patients with specific, chronic conditions, such as diabetes or CAD. Adding MARA brings patients to the surface who are most likely to be impactable in better clinical outcomes, lower costs or both. This is a very powerful way to prioritize your scarce and valuable care manger time.
In conclusion, the suite of groupers available in the MedInsight Ecosystem are each designed to serve a specific primary purpose and complement each other for patient or population level analysis. However, some of these tools can provide meaningful insight even outside of their primary application. For each project or initiative you should choose the grouper within your toolkit that is the best match for the desired application.
