Are you ready for HEDIS 2025? Streamline your workflows with an integrated risk adjustment solution
Every year, the National Committee for Quality Assurance (NCQA) publishes a detailed list of updates, additions, and deletions for the Healthcare Effectiveness Data and Information Set (HEDIS®).1As one of the most critical sets of performance measures in the healthcare industry, annual HEDIS changes are designed to reflect the improvement of patient care standards and have a profound impact on how organizations are scored and compared.
In this article, we will review those HEDIS measures that will be introduced, modified, and retired this year. We will also explore how a complete risk adjustment solution, which includes robust clinical documentation and streamlined workflows, can optimize outcomes and ensure compliance with the new standards. By understanding these changes and implementing a comprehensive risk adjustment strategy, healthcare organizations can not only meet regulatory requirements but also enhance the quality of care they provide to their patients.
What’s new in HEDIS 2025: A quick overview
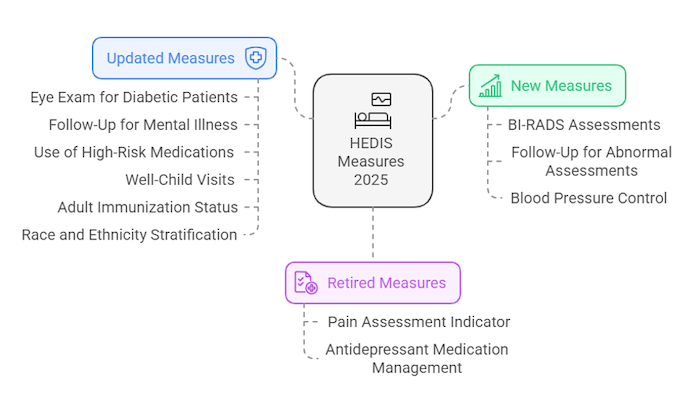
HEDIS is the measurement tool used by the nation’s health plans to evaluate their performance in terms of clinical quality and customer service. For Measurement Year (MY) 2025, NCQA is introducing three new HEDIS measures, retiring four measures, and adjusting several others.2 NCQA is also continuing the transition to Electronic Clinical Data Systems (ECDS) reporting.
Key changes include:
- New HEDIS Measures: The 2025 edition of HEDIS brings two additions to HEDIS focus on Breast Imaging Reporting and Data System (BI-RADS) assessments: Documented Assessment After Mammogram and Follow-up for Abnormal Breast Cancer Assessments. Also added for 2025 is Blood Pressure Control for Patients with Hypertension. All these measures use the ECDS reporting method, which leverages the extensive information available in electronic datasets used for patient care and quality improvement.
- Retired HEDIS Measures: To reduce burden and improve HEDIS, NCQA is retiring the Antidepressant Medication Management measure and Pain Assessment indicator in the Care for Older Adults measure. NCQA will monitor new evidence and is developing a chronic pain measure focused on older adults in the future. In addition, NCQA has a more comprehensive set of measures for depression screening, follow-up, routine monitoring, and outcome improvement.
- Changes to Existing HEDIS Measures: For MY 2025, NCQA has made several changes to existing HEDIS measures including: Eye Exam for Patients With Diabetes, Follow-Up After Emergency Department Visit for Mental Illness and Follow-Up After Hospitalization for Mental Illness, Use of High-Risk Medications in Older Adults, Well-Child Visits in the First 30 Months of Life and Child and Adolescent Well-Care Visits, Acute Hospital Utilization and Adult Immunization Status and Chlamydia Screening, and Race and Ethnicity Stratification (RES).
How risk adjustment impacts HEDIS performance
Risk adjustment can greatly improve HEDIS performance by helping healthcare organizations accurately assess and manage their patient populations, especially those with complex health needs. HEDIS measures evaluate the effectiveness of care in areas like preventive services, follow-up visits, chronic disease management, and mental health. Whereas risk adjustment measures the health status and demographic characteristics of patients.
However, both the HEDIS measures and the risk adjustment process involve collecting extensive data, which can be time-consuming and resource-intensive, and without the right processes can lead to data inconsistencies and lost revenue.
Common challenges include:
- Inefficient documentation and diagnosis coding: Errors in documenting and diagnosis coding can cause incorrect risk score calculations and potential Centers of Medicare and Medicaid Services (CMS) audit failures. Providers often struggle to ensure all relevant conditions are properly documented and coded, affecting both risk score accuracy and patient care quality measures.
- Incomplete or inaccurate risk scoring: Incomplete or incorrect risk scores can result in significant financial losses for Medicare Advantage plans and ACOs participating in Medicare Shared Savings Program (MSSP), ACO REACH, and other risk programs. This is because reimbursements from the CMS and other programs (e.g., ACA) are directly tied to these scores. Inaccurate scores can lead to lower reimbursements, impacting financial stability and the ability to invest in quality care.
- Undocumented or untreated conditions: Conditions that are not documented or treated can lead to missed care opportunities and lower reimbursements. A robust system to identify and address these gaps is crucial for high-quality care and financial efficiency.
To succeed in a value-driven market, organizations need a reliable, streamlined approach to gather information from electronic health records (EHRs), claims data, and other sources, and effectively bridge gaps in care and coding.
Milliman MedInsight: Your partner in risk & quality management
The Milliman MedInsight® Risk Adjustment Platform offers a comprehensive end-to-end solution that integrates industry expertise and proven technology with clinical documentation and workflows to enhance care, reduce costs, and manage financial risks. With this platform, your organization can confidently track its performance and meet the needs of each market: MA, MSSP, ACO REACH, Medicaid, commercial group, and ACA/individual markets.
With the Risk Adjustment Platform, your organization can:
- Streamline risk adjustment and quality processes: Drive successful risk adjustment initiatives and improve quality measurement. We seamlessly retrieve, scan, and process medical records from various sources into electronic medical record (EMR) systems, ensuring you have accurate and timely data at your fingertips to maximize the impact of each visit and intervention.
- Ensure accuracy and compliance: Maximize your data’s potential with our integrated risk adjustment solution. Our advanced retrospective and prospective processes provide a more accurate and complete view of your population’s health status, accelerating chart reviews, identifying conditions for recapture, and closing care gaps.
- Enhance clinical documentation, coding, and care: Ensure accurate records and identify opportunities to engage providers. Our approach corrects past coding errors for proper reimbursement and leverages real-time data to identify high-risk members early, enabling timely interventions to prevent issues and reduce healthcare costs.
Furthermore, our integrated Risk Adjustment Platform supports multiple teams within your organization, including:
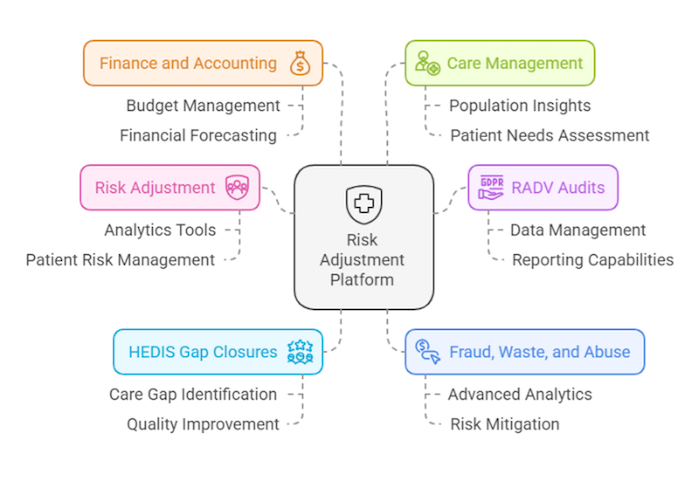
When data is leveraged effectively across the enterprise, your organization can more efficiently pinpoint areas needing improvement and implement strategies to boost performance scores. This proactive approach ensures compliance with regulations, helps avoid financial penalties, and most importantly improves patient outcomes.
Additional Risk Adjustment Platform resources
Schedule a call: Connect with one of our healthcare analytics experts.
Visit our website: Learn more about our Risk Adjustment Platform, a comprehensive, end-to-end risk adjustment solution.
Watch the webinar: Register to attend our upcoming webinar “Integrated risk adjustment solutions: Enhancing reimbursement and patient care” and learn how to optimize risk adjustment, RADV audits, and HEDIS gap closures.
Visit us at RISE: Connect with us at the RISE National 2025 conference held from March 11-14, 2025, in San Antonio.
References:
1. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
2. HEDIS MY 2025: What’s New, What’s Changed, What’s Retired – NCQA
